Gastrointestinal
M otility and Secretory Functions of the Alimentary Trac 10
M astication (Chewing)
Functions
Lubricate bolus with salivary secretion
Breakdown bolus to small particles
Begin digestion of carbohydrate ( α-amylase)
especially important for fruits and raw vegetables becauseindigestible cellulose membranes around their nutrient
portions
T eeth organization
Anterior teeth (incisors)
Posterior teeth (molars)
Chewing muscles are innervated by 5th
cranial nerve.
Chewing process is controlled by nuclei
in the brain stem.
Much of the chewing process is caused
by chewing & stretch reflexes
Presence of a bolus of food in the mouth initiates
reflex inhibition of muscles of mastication
causing
lower jaw to drop.
initiates a stretch reflex of jaw muscles
leading to rebound contraction.
which automatically raises the jaw to cause closure
of the teeth, and compresses the bolus against the
linings of the mouth
inhibits the jaw muscles
once again
allowing the jaw to drop and rebound
another time; this is repeated again and again.
S wallowing (Deglutition)
is the ordered sequence of events that
propels food from mouth to stomach
It is initiated voluntarily in the mouth, but thereafter is
under involuntary or reflex control.
The reflex portion is controlled by the swallowing
center in the medulla.
Stages of Swallowing:
Oral stage (voluntary)
Pharyngeal stage (involuntary)
Sensory impulses from the mouth
received by
nucleus tractus solitarius (NTS)
via medulla oblongata through trigeminal and glossopharyngeal Nerves.
The motor impulses to the pharynx and upper
esophagus are transmitted
from the swallowing
center by the 5th, 9th, 10th, and 12th cranial nerves
Esophageal stage (involuntary)
T he Swallowing process

1. Oral phase 2. Pharyngeal phase 3. Esophageal phase
Fu nction of Gastroesophageal Sphincter
This sphincter remains tonically constricted
(protects the esophagus from the stomach acidic
juices)
until the peristaltic swallowing wave passes
down the esophagus and causes a “receptive
relaxation” of the sphincter
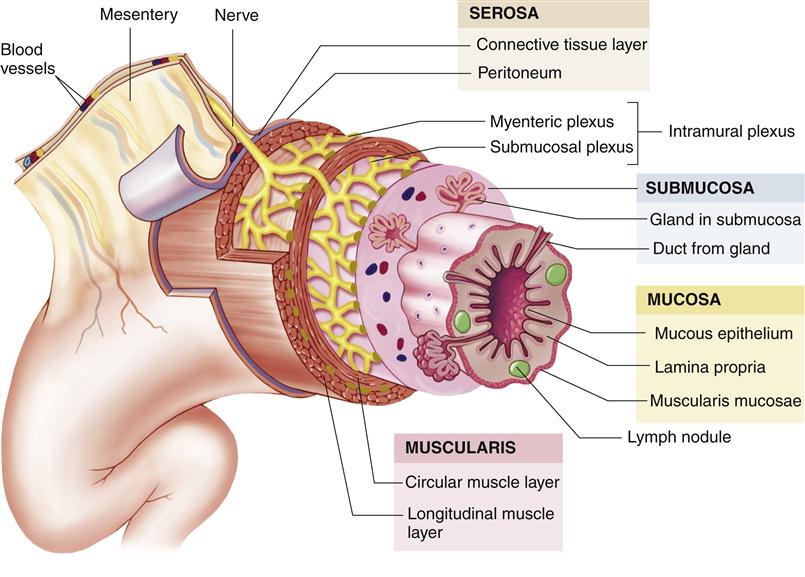
Physiological Anatomy of the GIT Wal 1
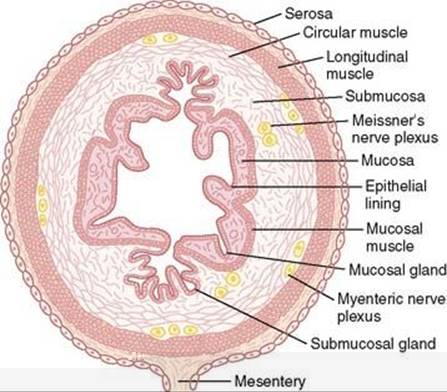
.
.
Longtitudinal.m it's contraction causes shorting.
Circular.m it's contraction causes an increase in luminal pressure
Neural Control of Gastrointestinal Function 6
Enteric Nervous System (ENS):
Is the nervous system of GI
tract + lies entirely in the wall of
the gut
has as many neurons
(about 100 million).
composed mainly of two plexuses
Outer
Lying between
longitudinal and circular
muscle layers
Called myenteric or
Auerbach’s plexus
Controls mainly GI
movements.
Inner
Lying in the submucosa
• called the submucosal
or Meissner's plexus
controls mainly GI
secretion, absorption
and local blood flow.

On GIT wall
SMOOTH MUSCLE CLASSIFICATIONS 2
Unitary type (single unit):
Numerous smooth muscle fibers
that contract together as a single
unit.
Cells are electrically coupled via
gap junctions
Multiunit type:
Composed of separate smooth muscle fibers.
•Each fiber operates
independently with single nerve ending
Contract in response to neural
input (such as in esophagus &
gall bladder)

Subtopic

Types of Neurotransmitters Secreted byENs 7
Excitatory motor neurons:
evoke muscle contraction &
intestinal secretion
Neurotransmitters of motor neurons
Substance P
Ach (acetylcholine)
Neurotransmitters of secreto-motor neurons
Release of water, electrolytes and mucus from crypts of Lieberkuhn
Ach
VIP (vasoactive intestinal peptide)
Histamine
Inhibitory motor neurons
suppress muscle contraction
ATP
NO (nitric oxide)
VIP
TYPES OF CONTRACTION 3
Phasic contractions
Periodic contractions
followed by relaxation
Such as in gastric
antrum, small intestine
and esophagus
Associated with slow
waves
Tonic contractions
Continuous contraction without
relaxation
Such as in Orad region of stomach,
lower esophageal, ileocecal and
internal anal sphincter
Caused by:
repetitive spike
potentials
hormones
entry of
Ca ions (not associated with
changes in membrane potentials)
main smooth muscle layer 4
Longitudinal (A)
• Contraction shortens length
expands lumen of longitudinal.
• Innervated by enterics
nervous system (ENS), mainly by excitatory
motor neurons.
Circular (B)
Thicker and more
powerful
Contraction reduces
lumen and increases
length.
• Innervated by ENS, both Excitatory and inhibitory
motor neurons.
More gap junctions.
Types of Movements in the GI 9
propulsive
cause food to move
forward along the
tract at an appropriate
rate
to accommodate
digestion and
absorption
Basic movement in gitis peristalsis
Usual stimulus is distention
Other stimuli
chemical
physical irritation of
epithelial lining in gut.
Atropine (cholinergic blocker) depresses propulsion
Myenteric plexus is important for peristalsis
Parasympathetic stimulation
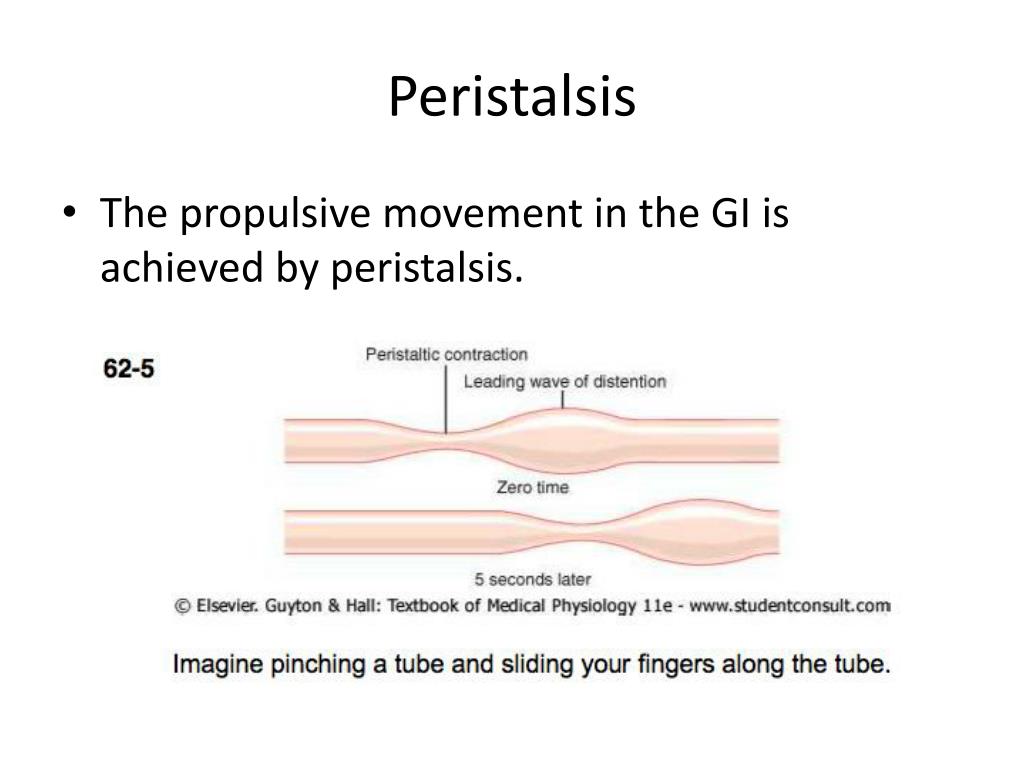
The gut can cause a contractile ring to
appear in the circular muscle, and this ring then spreads along the gut tube.
mixing(segmentation
keep the intestinal
contents thoroughly
mixed at all times

Subtopic
Blend different juices
with the chyme.
Bring products of
digestion in contact
with absorptive
surfaces.
Hormonal control

.
Specific Characteristics of Smooth Muscle in the Gut 5
Functions as syncytium
Individual smooth muscle fibers are arranged in bundles
each bundle, muscle fibers are electrically connected
through large numbers of gap junctions.
Each muscle layer functions as a syncytium
Start of A.P anywhere within muscle it travels to all directions in muscle
Electrical Activity of it
Smooth muscle of the GIT is excited by continual slow
intrinsic
It has 2 basic types of electrical waves:
Slow waves
Most GI contractions occur rhythmicall
determined by ferquency of the “slow waves“ of s.m membrane potential
Are not A.P
They are oscillating depolarization and repolarization in
the resting membrane potential with unknown cause.
Their intensity varies (5 -15 mv)
Frequency (from 3 to 12 /min):
3 in body of stomach
12
in duodenum
8 terminal ileum
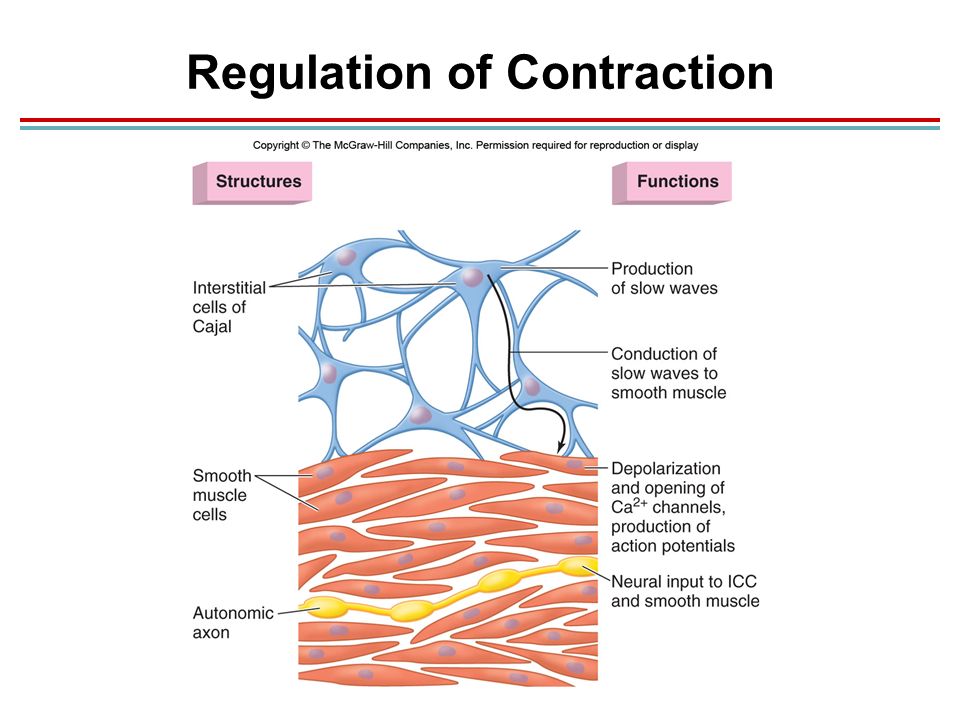
O rigin of slow waves
From interstitial cells of Cajal
ICC, the GI pacemaker), which are abundant in the myenteric
plexuses.
ICCs form a network with each other
interposed
between the smooth muscle layers
with synaptic-like
contacts to smooth muscle cells.

Subtopic
Subtopic
spikes
are true action potentials
Occur automatically
when resting membrane potential
of GIT smooth muscle becomes more positive
(-40mV) (normal resting membrane potential is
between -50 and -60 mV).
slow wave potential rises there is a greater
frequency of spike potentials
potentials excite the muscle contraction.
Autonomic Control of the Gastrointestinal Tract 8
Parasympathetic
Stimulates GIT
Activity.
Innervation
C ranial
entirely In vagus nerve.
esophagus, stomach, pancreas and the intestines down to the first half of the large intestine.
Sacral
pelvic nerves
distal half of the large intestine up to anus (to execute defecation reflexes).
Sympathetic
Inhibits GIT Activity.
fibers originate in spinal cord
between segments T-5 and L-2 To git
Innervate essentially all of the GI tract.
It's ending secrets norepinephrine